BIMONTHLY INTERNAL ASSESSMENT - DECEMBER
- Get link
- X
- Other Apps
1) A 55 year old man with Recurrent Focal Seizures
Detailed patient case report here: http://ushaindurthi.
1. What is the problem representation of this patient and what could be the anatomical site of lesion ?
A 55 year old male construction worker with T2DM who is a chronic alcoholic & smoker came with c/o weakness of right upper limb with involuntary movements of both right UL & LL secondary to ? right temporal lobe epileptogenic focus.
2. Why are subcortical internal capsular infarcts more common that cortical infarcts?
subcortical infarcts are caused by occlusion of a penetrating artery from a large cerebral artery, most commonly from the Circle of Willis. These penetrating arteries arise at sharp angles from major vessels and are thus, anatomically prone to constriction and occlusion.
So subcortical infarcts are more common than cortical infarcts.
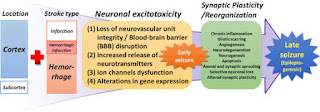
3. What is the pathogenesis involved in cerebral infarct related seizures?
4. What is your take on the ecg? And do you agree with the treating team on starting the patient on Enoxaparin?
ST depressions noted in precordial leads V1 to V6
Yes , i agree with the treating team on starting the patient on Enoxaparin.
5. Which AED would you prefer?
Please provide studies on efficacies of each of the treatment given to this patient.
As it is focal seizure i would prefer carbamazepine
Questions:
1. What is the problem representation for this patient?
Pulmonary function abnormalities resulting from obesity
4. What is the pathogenesis involved in hypoglycemia ?
5. Do you agree with the treating team on starting the patient on antibiotics? And why? Mention the efficacies for the treatment given.
3(A)
Case details here: https://
1. How would you evaluate further this patient with Polyarthralgia?
2. What is the pathogenesis involved in RA?
3. What are the treatment regimens for a patient with RA and their efficacies?
The following abbreviations and nomenclature for disease-modifying antirheumatic drugs (DMARDs) were used in this document:
csDMARD: conventional synthetic disease-modifying antirheumatic drugs - methotrexate, leflunomide, sulfasalazine, and antimalarial drugs (hydroxychloroquine and chloroquine).
tsDMARD: synthetic target-specific disease-modifying antirheumatic drug - tofacitinib.
bDMARD: biological disease-modifying antirheumatic drugs - tumor necrosis factor inhibitors/TNFi (adalimumab, certolizumab, etanercept, golimumab, infliximab), T-lymphocyte co-stimulation modulator (abatacept), anti-CD20 (rituximab), and IL-6 receptor blocker (tocilizumab).
boDMARD: original biological disease-modifying antirheumatic drugs.
bsDMARD: biosimilar biological disease-modifying antirheumatic drugs.
Efficacy and safety of various anti-rheumatic treatments for patients with rheumatoid arthritis:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6348345/
3(B)75 year old woman with post operative hepatitis following blood transfusion
Case details here: https://
1.What are your differentials for this patient and how would you evaluate?
coombs testing
antibody panel testing
-Post transfusion hepatitis
2. What would be your treatment approach? Do you agree with the treatment provided by the treating team and why? What are their efficacies?
- Lasix & Nebulization : For wheezing and crepts
- Lactulose : To prevent hepatic encephalopathy https://pubmed.ncbi.nlm.nih.gov/27089005/
- Zofer : For vomitings
- Pantop : To prevent gastritis
http://manojkumar1008.
1. What is the problem representation of this patient?
A 60 year old female with T2DM c/o pricking type of chest pain since 4 days and uncontrolled sugars secondary to ? right upper lobe pneumonic consolidation with sepsis
2. What are the factors contributing to her uncontrolled blood sugars?
Hyperdense area noted in the right upper lobe
4. What do you think is the cause for her hypoalbuminaemia? How would you approach it?
- Inflammation (acute phase reactant)
- Malnutrition
- Albuminuria (protein losing nephropathy)
- Piptaz & clarithromycin : for his right upper lobe pneumonic consolidation and sepsis
- Egg white & protien powder : for hypoalbuminemia
- Lactulose : for constipation
- Actrapid / Mixtard : for hyperglycemia
- Tramadol : for pain management
- Pantop : to prevent gastritis
- Zofer : to prevent vomitings
Case report here: https://appalaaishwaryareddy.
1. What is the anatomical and pathological localization of the problem?
2. How do you approach and evaluate this patient with Hepatitis B?
3. What is the pathogenesis of the illness due to Hepatitis B?
4. Is it necessary to have a separate haemodialysis set up for hepatits B patients and why?
Yes , separate machines must be used for patients known to be infected with HBV (or at high risk of new HBV infection). A machine that has been used for patients infected with HBV can be used again for non-infected patients only after it has been decontaminated using a regime deemed effective against HBV because of increased risk of transmission due to contamination.
5. What are the efficacies of each treatment given to this patient? Describe the efficacies with supportive RCT evidence.
- Lactulose : for prevention and treatment of hepatic encephalopathy. https://pubmed.ncbi.nlm.nih.gov/27089005/
- Tenofovir : for HBV
- Lasix : for fluid overload (AKI on CKD) https://www.ncbi.nlm.nih.gov/books/NBK499921/#:~:text=The%20Food%20and%20Drug%20Administration,failure%20including%20the%20nephrotic%20syndrome.
- Vitamin -k : for ? Deranged coagulation profile (PT , INR & APTT reports not available)
- Pantop : for gastritis
- Zofer : to prevent vomitings
- Monocef (ceftriaxone) : for AKI (? renal)
6) 58 year old man with Dementia
Case report details: http://
1. What is the problem representation of this patient?
A 58 year old weaver occasional alcoholic c/o slurring of speech , deviation of mouth to right side associated with drooling of saliva , food particles and water predominantly from left angle of mouth and smacking of lips since 6 months.
2. How would you evaluate further this patient with Dementia?
4. What is the likely pathogenesis of this patient's dementia?
(1) Neurotoxicity, including dysregulated glutamate and calcium signaling, and neurotransmission imbalance contribute to synaptic dysfunction and neuronal loss
(2) Glia activation, including microglia and astrocytes, interfere with immunological processes in the brain further promoting non-resolving inflammation and neurodegeneration
(3) Tau phosphorylation and neurofibrillary tangle formation;
(4) Aβ plaque formation are key hallmarks of the AD brain. Specialized pro-resolving mediators and strategies aimed at boosting resolution such as using omega-3 polyunsaturated fatty acid exert differential effects on these targets and provide anti-inflammatory and pro-cognitive effects in neuroinflammation/degeneration
(5) The accumulation of Aβ may lead to the microglial accumulation and activation resulting in increases in pro-inflammatory cytokines such as interleukin-1 beta, interleukin-6, and tumor necrosis factor-alpha. These cytokine increases in the brain can subsequently lead to tau hyperphosphorylation and a pathological cycle of increased Aβ deposition and persistent microglial activation, ultimately resulting in chronic neuroinflammation and neurodegeneration.
5. Are you aware of pharmacological and non pharmacological interventions to treat such a patient and what are their known efficacies based on RCT evidence?
- Donepezil
- Rivastigmine
- Galantamine
- Memantine
- Counselling the patient and care givers
- Geriatric care
- Cognitive / emotion oriented interventions
- Sensory stimulation interventions
- Behaviour management techniques
7) 22 year old man with seizures
Case report here http://geethagugloth.
1. What is the problem representation of this patient ? What is the anatomic and pathologic localization in view of the clinical and radiological findings?
2. What the your differentials to his ring enhancing lesions?
3. What is "immune reconstitution inflammatory syndrome IRIS and how was this patient's treatment modified to avoid the possibility of his developing it?
A paradoxical clinical worsening of a known condition or the appearance of a new condition after initiating anti retroviral therapy (ART) therapy in HIV-infected patients resulting from restored immunity to specific infectious or non-infectious antigens is defined as immune reconstitution inflammatory syndrome (IRIS).
As his CD4 count is > 50 /mm3 consider delayed initiation of ART ideally after 8 weeks of starting ATT to reduce the chances of developing IRIS
- Transfusion reactions
- Cardiorenal association in different way
- Dialysis on daily basis / CRRT dialysis
- Unexplained delirium due to malnutrition / sepsis
- No rise in Hb after blood transfusion which can be attributed to various factors that lead to RBC destruction during storage
- Role of prophylactic anticoagulant usage in AF
- Hypertensive urgency management
- Status epilepticus management
- Get link
- X
- Other Apps